Hello, I'm
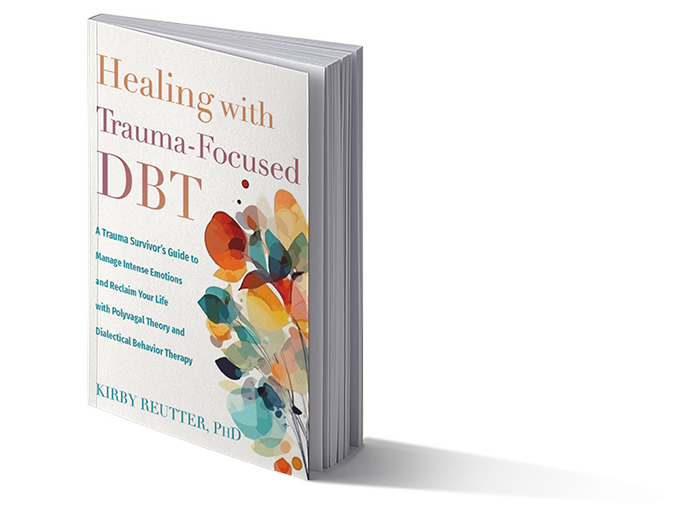
Dr. Kirby Reutter
MSCP, CDBT, LMHC, MAC, etc
"When trauma strikes, we are leveled, reduced to ashes, knocked out, and brought to our knees. We hit our rock bottom. We meet our ground zero. In short, we do not start our journey feeling like a hero. But this journey is the only way that heroes are made." - Dr. Reutter, Healing with Trauma-Focused DBT, page 162
You Can Click Below to Order
SERVICES

Adoption Evaluations
Dr. Reutter provides prompt, expert evaluations for couples pursuing international adoption.

Trauma Treatment
Dr. Reutter provides expert, best
practice treatment services for
survivors of trauma.

DBT Trainings
Dr. Reutter provides expert, cross-continental trainings in Dialectical Behavior Therapy.
Earn CEU's
Dr. Reutter provides 18 hours of CEU’s through an expert interview series and 2 courses on Trauma-Focused DBT.
IN THE MEDIA

Call Us Today
512.788.5611
FROM THE BLOG
Stay current on blogs related to PTSD and trauma.

What Is Trauma? Part 2
To this day, many medical professionals do not fully understand or appreciate the physical impact of trauma on the nervous system (and therefore, the entire body). Since the nervous system interacts w...
Read More
What Is Trauma? Part 1
Trauma affects every part of the body and every part of the brain. That’s a lot of turf. There is still much that even highly trained professionals do not understand about how trauma affects a person,...
Read More
DBT and Trauma: Part 2
Dialectical behavior therapy (DBT) was developed in the 1970s by Dr. Marsha Linehan to treat symptoms of what we call borderline personality disorder. A borderline personality is characterized by a fe...
Read More



